Rhinoplasty
Rhinoplasty, which is often referred to as a nose job, is a plastic surgery procedure that alters the reconstructs the nose for cosmetic or functional reasons. A reconstructive Rhinoplasty surgery that corrects the form and functions of the nose, while a cosmetic Rhinoplasty surgery that alters the appearance of the nose.
We commonly are asked by patients to correct a nasal problem such as breathing difficulties. This is a functional problem. Other patients do not like their appearance and request visual improvements. This a cosmetic problem. We will be discussing, in general terms, the correction of problems in both of these areas.
Rhinoplasty FAQs
Written and reviewed by:
This article was written by Dr. Vincent Zubowicz, who is board certified by the American Board of Plastic and Reconstructive Surgery. He practices medicine at his offices in Milton and Atlanta. Learn more about Dr. Zubowicz, his medical training, and credentials.
Customer Reviews

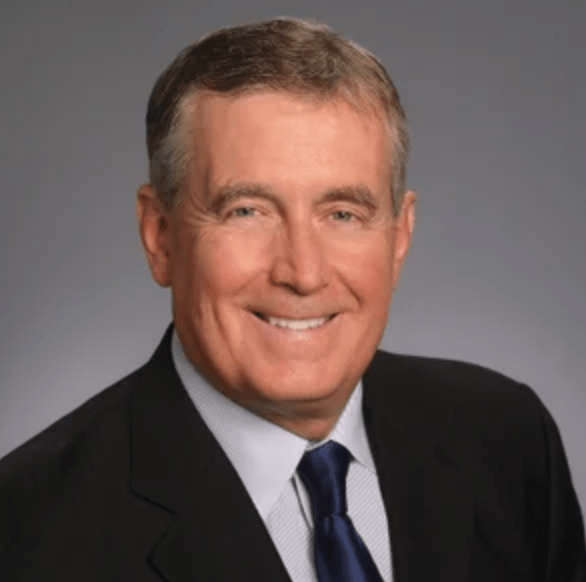
Dr. Vincent Zubowicz is one of the Atlanta areas top plastic and reconstructive surgeons. He is an expert in cosmetic surgery, with years of experience performing many plastic surgery procedures. He offers a personal, customized approach and is dedicated to helping patients achieve the most natural looking results.
Call our office at 470-462-2917 to schedule your consultation with Dr. Vincent Zubowicz.